Affiliated Research Teams
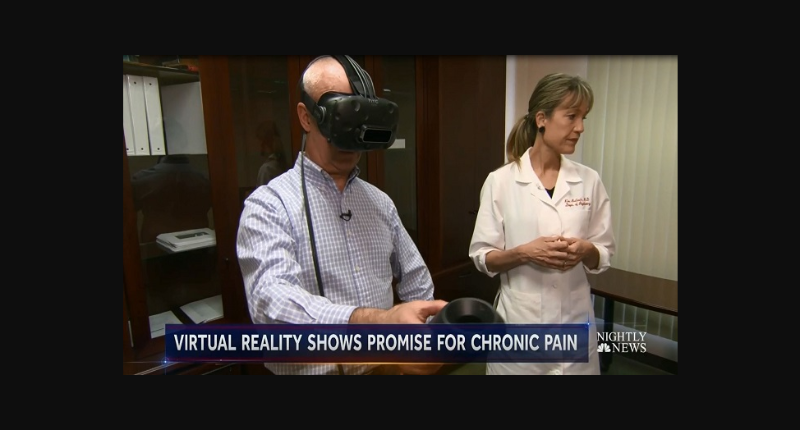
Kim Bullock, M.D.
The Virtual Reality & Immersive Technology (VR-IT) Program at Stanford honors the creative, collaborative, and innovative spirit of our psychiatry department thru the unconventional and interdisciplinary development, evaluation, and dissemination of immersive technology based treatments. This program is guiding and safe-guarding the evolution of technology ‘s inevitable merging with the human nervous system in the service of behavioral and mental health. With the development of biometric sensing devices, virtual reality and perceptual illusions can now provide sensory feedback experiences relevant to permanently changing psychiatric illnesses. The use of these break-thru technologies allows precise and personalized shaping and conditioning of behavior which can be customized to unique individuals and circumstances.
CONNECTING: The VR-IT program was founded by neuropsychiatrist Kim Bullock for the purpose of supporting the projects of individuals developing immersive technologies with the aim of relieving suffering and increasing emotional wellbeing. The VR-IT program is a leader and a disrupter in providing support and connecting researchers, providers, and industry stakeholders thru networks of communication facilitated by its auxiliary organization the Stanford Psychiatry Immersive Technology Consortium (SPITC).
EDUCATING: The VR-IT program serves to disseminate rapidly changing and emerging technology therapies by training clinicians in evidenced based VR interventions thru one-on-one supervision, workshops, and CME conferences.
EXPLORING: Dr. Bullock’s primary area of research is multimodal treatments for illnesses that involve dysregulation of bodily sensations and functions. She is currently focusing on the use of embodied virtual reality technology to augment physiotherapy, psychotherapy, and skills acquisition for somatic symptom related disorders.
E-mail | Stanford Profile | Clinical Trials | VR-IT Lab | Stanford Neurosciences Institute
Collaborators: Andrea Won, Ph.D., Jeremy Bailenson, Ph.D., Katharine Dahl, M.D., Walter Greenleaf, Ph.D., Antonio Hardan, M.D., Kate Hardy, Clin.Psych.D., Chariot, Elizabeth McMahon, Ph.D., Hadi Hosseini, Ph.D., Carolyn Rodriguez, MD, PhD, Samuel Rodriguez, MD, Lauren Mikula Schneider, M.D., Debra Safer MD, Sarah Adler, Psy.D., Cristin Runfola, PhD, Nina Vasan, M.D. Ryan Matlow, Ph.D., Pam Shime, J.D.